
Technical Volume 1:
Cybersecurity Practices
for Small Healthcare
Organizations
2023 Edition

iTechnical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Table of Contents
Introduction 1
Where Can You Go for Addional Resources? ........................................................................................................................................2
What are Managed IT Services? ..................................................................................................................................................................... 3
Different Types of Managed IT Services ................................................................................................................................................... 3
How Do I Select a Vendor? ................................................................................................................................................................................. 4
Document Guide: Cybersecurity Practices 7
Cybersecurity Practice #1: Email Protection Systems 9
Sub-Pracces for Small Organizaons .......................................................................................................................................................... 9
1.S.A: Email System Conguration................................................................................................................................................................ 9
1.S.B: Education
......................................................................................................................................................................................................10
1.S.C: Phishing Simulations .............................................................................................................................................................................11
Key Migated Threats ............................................................................................................................................................................................ 12
Cybersecurity Practice #2: Endpoint Protection Systems 13
Sub-Pracces for Small Organizaons .......................................................................................................................................................13
2.S.A: Basic Endpoint Protection Controls ...........................................................................................................................................13
Key Migated Threats ............................................................................................................................................................................................ 15
Cybersecurity Practice #3: Access Management 16
Sub-Pracces for Small Organizaons .......................................................................................................................................................16
3.S.A: Basic Access Management ................................................................................................................................................................16
Key Migated Threats ............................................................................................................................................................................................ 18
Cybersecurity Practice #4: Data Protection and Loss Prevention 19
Sub-Pracces for Small Organizaons .......................................................................................................................................................19
4.S.A: Policies ............................................................................................................................................................................................................19
4.S.B: Procedures ...................................................................................................................................................................................................20
4.S.C: Education ...................................................................................................................................................................................................... 21
Key Migated Threats ............................................................................................................................................................................................ 21
Cybersecurity Practice #5: Asset Management 22
Sub-Pracces for Small Organizaons .......................................................................................................................................................22
5.S.A: Inventory .......................................................................................................................................................................................................22
5.S.B: Procurement ...............................................................................................................................................................................................23
5.S.C: Decommissioning ................................................................................................................................................................................... 23
Key Migated Threats ............................................................................................................................................................................................ 23
Cybersecurity Practice #6: Network Management 24
Sub-Pracces for Small Organizaons .......................................................................................................................................................24
6.S.A: Network Segmentation .......................................................................................................................................................................24
6.S.B: Physical Security and Guest Access ............................................................................................................................................25
6.S.C: Intrusion Prevention .............................................................................................................................................................................25
Key Migated Threats ............................................................................................................................................................................................ 25

iiTechnical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Practice #7: Vulnerability Management 26
Sub-Pracces for Small Organizaons .......................................................................................................................................................26
7.S.A: Vulnerability Management ............................................................................................................................................................... 26
Key Migated Threats ............................................................................................................................................................................................ 26
Cybersecurity Practice #8: Incident Response 27
Sub-Pracces for Small Organizaons .......................................................................................................................................................27
8.S.A: Incident Response ..................................................................................................................................................................................27
8.S.B: Information Sharing ...............................................................................................................................................................................29
Key Migated Threats ............................................................................................................................................................................................ 29
Cybersecurity Practice #9: Network Connected Medical Devices 30
Sub-Pracces for Small Organizaons .......................................................................................................................................................30
9.S.A: Medical Device Security ..................................................................................................................................................................... 30
Key Migated Threats ............................................................................................................................................................................................ 30
Cybersecurity Practice #10: Cybersecurity Oversight and Governance 31
Sub-Pracces for Small Organizaons .......................................................................................................................................................31
10.S.A: Policies.........................................................................................................................................................................................................31
10.S.B: Cybersecurity Risk Assessment and Management
33.......................................................................................................
10.S.C: Security Awareness and Training .............................................................................................................................................. 35
10.S.D: Cyber Insurance ...................................................................................................................................................................................35
Key Migated Threats ............................................................................................................................................................................................ 36
Appendix A: Acronyms and Abbreviations 37
Appendix B: References 39
Tables
Table 1. Five Prevailing Cybersecurity Threats to Healthcare Organizaons 7...................................................................
Table 2. Cybersecurity Pracces and Sub-Pracces for Small Organizaons 7...................................................................
Table 3. Phishing Detecon ...............................................................................................................................................................................11
Table 4. Eecve Security Controls to Protect Organizaon Endpoints ...........................................................................13
Table 5. Security Controls Enabling Organizaons to Manage User Access to Data ................................................ 16
Table 6. Example Data Classicaon Structure ...................................................................................................................................20
Table 7. Roles and Responsibilies of an Incident Response Team 28.......................................................................................
Table 8. Eecve Policies to Migate the Risk of Cyber-Aacks 32...........................................................................................
Table 9. Acronyms and Abbreviaons .........................................................................................................................................................37

1Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Introducon
Healthcare providers are being attacked by malicious actors, some from inside their own organizations
and others from around the globe. While news reports may insinuate larger providers are targeted
more frequently, the data suggests smaller ambulatory practices are also targeted and can suffer greater
proportional damages. The rationale is that smaller providers are generally less prepared to detect,
respond, and recover from cyber-attacks.
Indeed, the ve threats identied in the Main Document can be very disruptive to small organizations. For
example, if a small provider practice loses a laptop with unencrypted Protected Health Information (PHI),
a publicized breach could result in consequences for the provider’s patients and the practice’s reputation.
Technical Volume 1 outlines healthcare cybersecurity best practices for small healthcare organizations.
For this volume, small organizations generally do not have dedicated information technology (IT) and
security staff dedicated to implementing cybersecurity practices. Consequently, personnel may have
limited awareness of the severity of cyber threats to patients and to your organization, and thus, not
recognize the importance of cybersecurity and how to address it.
Many small healthcare organizations provide direct healthcare services to their patients in ambulatory
environments. These environments have less overhead and, because of this, are often more cost-
effective than large acute facilities. Cost-effectiveness enables small healthcare organizations to sustain
operations, maintain nancial viability, justify future investments (e.g., grants) and, in the case of for-
prot organizations, generate an acceptable prot. Conducting day-to-day business usually involves the
electronic sharing of clinical and nancial information. This is done internally within the small healthcare
organization and its physicians and externally with patients, providers, and vendors that have a role
in managing your organization and maintaining business operations. For example, small healthcare
organizations transmit nancial information to submit invoices and insurance claims paid by Medicare,
Medicaid, Health Maintenance Organizations (HMOs), and commercial insurance companies.
In general, small organizations perform the following functions:
• Clinical care, which includes but is not limited to sharing information for clinical care, transitioning
care (both social and clinical), electronic prescribing or “e-prescribing,” communicating with
patients through direct secure messaging, services provided through telehealth, and operating
diagnostic equipment connected to a computer network (e.g., ultrasound and picture archiving and
communication systems (PACS)).
• Provider practice management, which includes patient access and registration, patient accounting,
patient scheduling systems, claims management, and bill processing.
• Business operations, which include accounts payable, supply chain, human resources, IT, staff
education, protecting patient information, and business continuity/disaster recovery.
If you would like to conrm your status as a small healthcare organization, refer to the HICP Main
Document, Table 1.
Just as healthcare professionals must wash their hands before caring for patients, healthcare
organizations must practice good cyber hygiene by including cybersecurity as an everyday, universal
precaution. Like hand washing, cyber awareness does not have to be complicated or expensive. In fact,
simple cybersecurity practices, such as always logging off a computer when nished working, are very
effective at protecting sensitive information.
Introduction
2Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
This volume takes into consideration regulations, guidance, and best practice recommendations made
by the U.S. Department of Health & Human Services (HHS) and its operating divisions and staff divisions.
Operating divisions and staff divisions include, but are not limited to, the Ofce for Civil Rights (OCR),
the Food and Drug Administration (FDA), the Administration for Strategic Preparedness and Response
(ASPR), the Ofce of the Chief Information Ofcer (OCIO), the Centers for Medicare and Medicaid
Services (CMS), and the Ofce of the National Coordinator for Health Information Technology (ONC).
Other recommendations are derived from guidelines and leading practices from the National Institute of
Standards and Technology (NIST), the Department of Homeland Security (DHS), and the Cybersecurity
and Infrastructure Security Agency (CISA).
Many small healthcare organizations use third-party IT support and cloud service providers to maintain
operations that leverage current technologies. Given the complicated nature of IT and cybersecurity,
these third-party IT organizations can be helpful in identifying, assessing, and implementing cybersecurity
practices. Your IT support providers should be capable of reviewing the practices in this publication to
determine which are most applicable to your organization.
In addition to IT requirements, small healthcare organizations must comply with multiple legal and
regulatory standards as well as contractual agreements. Healthcare practices often ensure compliance
by creating an internal infrastructure of personnel and procedures governing how they safeguard the
maintenance and transmission of sensitive data. Organizations may be subject to directives from:
• Information blocking and interoperability regulations for patient information mandated by the ONC
Cures Act Final Rule.
• Medicare Access and the Children’s Health Insurance Program (CHIP) Reauthorization Act of 2015
(MACRA)/Meaningful Use.
• Privacy and Security Rules of the Health Insurance Portability and Accountability Act (HIPAA)/
Health Information Technology Economic and Clinical Health Act (HITECH).
• Payment Card Industry Data Security Standard (PCI-DSS).
• Substance Abuse and Mental Health Services Administration (SAMHSA) regulations for the
condentiality of substance abuse disorder treatment records (42 CFR Part 2).
• Changes to the Stark Law physician self-referral regulations and the related anti-kickback safe
harbor took effect in 2021, allowing for the donation of cybersecurity technology and necessary
services used predominantly to implement, maintain, and reestablish effective cybersecurity.
• State law requirements for maintaining patient treatment records, as well as the safeguarding and
destruction of data containing health information.
Where Can You Go for Additional Resources?
The 405(d) Program and Task Group is a collaborative effort between industry and the federal
government, which aims to raise awareness, provide vetted cybersecurity practices, and move
organizations towards consistency in mitigating the current most pertinent cybersecurity threats to the
sector. Please explore the 405(d) website to learn more about all products and resources available to
our stakeholders.
CISA has published the CISA Services Catalog, which is intended to serve as a single touch point
for anyone interested in CISA’s services. An interactive section of this resource allows health care
organizations to quickly focus on the services that best t their capabilities and challenges, based on

Introduction
3Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
their characteristics and maturity level. For example, healthcare providers can select services they’re
interested in across four categories—cybersecurity, risk management, infrastructure, and emergency
communications—then choose their readiness level. After these selections, they are then presented with
all the CISA services most appropriate for them. Also in the resource, users can access and peruse all CISA
service indices and understand how CISA’s staff is organized and distributed throughout the country.
For additional resources please visit 405(d), OCR, HC3, NIST, and FBI.
Types of Managed Services in Health IT
The scope and breadth of information technology in healthcare has evolved rapidly in the twenty-rst
century. Health-IT is a critical component of almost every healthcare organization. Electronic health
records (EHRs), medical devices, and business management software applications have been integrated
into clinical practice and health care operations.
However, for various reasons, not all healthcare organizations have the resources to build out a team
of experts to operate or maintain their information technology assets. This is especially true for small
healthcare organizations. To meet EHR use, health information exchange, and other IT requirements,
many healthcare organizations depend on managed IT services from an outside vendor.
What are Managed IT Services?
Managed IT services (outsourced IT) is a third-party service that provides infrastructure, IT, and other
technical support to healthcare organizations. These service providers are often referred to as a managed
service provider (MSP). To simplify our discussion, we will label all outsourced IT services of any size or
scope as being provided by an MSP vendor.
MSP service offerings vary widely, covering everything from cybersecurity needs, voice-over-internet-
protocol (VoIP), telehealth solutions, backup recovery, and integrated business activities. Healthcare
organizations often seek out MSP support because they cannot hire and manage an internal IT team, or
they prefer the expertise and exibility of contracted services.
As MSPs cover a broad range of many different types of managed services, it is important to understand
what each vendor includes when you are contracting services. Knowing what the service options are and
which ones your healthcare organization needs is an important rst step.
Different Types of Managed IT Services
There are various types of vendors and services available to healthcare organizations. Not all providers
will offer the same types of IT services. One MSP might be a small, locally based IT contractor that
provides a handful of services; or specializes in just one type of service. Other MSPs may seek to offer
a comprehensive selection of IT and security services to be the sole vendor for an organization’s IT
management needs. Regardless, if your healthcare organization wants to outsource its IT management, it
is good to know what services are offered and what services are included in your contract.
• Managed Networks and Infrastructure: With this type of service, an MSP generally takes on the
entirety of network tasks. This includes establishing internet connectivity, managing local wired
networks, and wireless networks plus various connections for your healthcare organization. They
may also manage data backup, recovery, and storage options.

Introduction
4Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
• Managed Security: A managed security service provider (MSSP) provides outsourced monitoring and
management of security devices and systems. Common services include managed rewall, intrusion
detection, virtual private network (VPN), vulnerability scanning, and malware prevention/anti-virus
tools. MSSPs will often conduct cybersecurity risk assessments, which is critically important for
HIPAA compliance. Some MSSPs provide consulting services for mitigating gaps identied through
the risk assessment.
• Managed Support and Help Desk Services: Typically provides all services related to IT help—
troubleshooting, resetting passwords, and dealing with advanced issues.
• Managed Print Services: With this type of managed service, an MSP will remotely assist with
document management, data and le infrastructure of multi-function devices, printers, and fax
machines. These services are most often used by organizations producing, receiving, and storing high
volumes of digital or printed documents.
• Managed Cloud Infrastructure: Cloud infrastructure management handles computing, storage,
network, and IT. Some vendors may also offer virtualization services for apps, software, operating
systems, or electronic health record systems.
• Managed Software as a Service (SaaS): With this type of service, vendors offer a software platform,
typically subscription-based, for healthcare organizations. A few examples include Microsoft 365,
Zoom, e-prescribing software, and anti-malware/anti-virus software.
• Managed Wireless and Mobile Computing: A vendor offering managed wireless and mobile computing
will implement wireless local-area network (WLAN) connections. Examples of wireless and mobile
computing are Wi-Fi networks internal to a healthcare facility, telehealth systems, and internet-of-
things (IoT) devices.
• Managed Communication Services: This type of service offers a range of communication infrastructure
like messaging software, VoIP telephone, data, and video. Examples are Ring, Zoom, and Skype.
• Data Analytics: Healthcare data analytics is the process of analyzing current and historical industry
data to predict trends, improve outreach, and better manage the spread of disease. It can reveal
paths to improvement in patient care quality, clinical data, diagnosis, and business management.
• Managed Electronic Health Record (EHR) and Practice Management: This type of service will manage
components of the main EHR and/or practice management suite. It could include ensuring the
maintenance of the EHR itself, updating workows, managing revenue cycle and billing, or other
clinical practice management needs.
How Do I Select a Vendor?
Vendor Assessment: Beginning Vendor Selection
A vendor assessment is the process of collecting information on several vendors and narrowing the
vendor eld before selecting an MSP. The challenge of narrowing a large eld of available options to a
manageable number of vendors can be daunting, but it is a critical step in outsourcing your IT.
Suggestions for Conducting an MSP Vendor Assessment
Follow the steps below to ensure your healthcare organization can conduct a vendor assessment
effectively and efciently.
Introduction
5Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
1. Assess Your IT Management Needs: Identify high priority needs and IT features that may meet those
needs. Make sure you identify what information network features you will need to achieve the goals
your organization requires for its information systems.
2. Set Information Technology Network Goals: Follow the “SMART” goals process. Goals should be
specic, measurable, attainable, relevant, and time bound.
3. Make Key Decisions: Make a list of potential deal-breakers and decide whether you want your
healthcare organization’s data to reside in-ofce, a vendor server, or in web-based storage (“cloud
storage”). To help form a list of potential deal-breakers, research vendor websites and speak to
colleagues. Making key decisions up-front will enable your practice to effectively narrow the eld.
4. Narrow the Field: You can start with vendor reviews and ratings for IT managed service providers
gathered from healthcare industry leaders. Leading reviews are aggregated and reported by
Gartner
1
and KLAS Research.
2
¡ Ask colleagues about their IT managed service provider experiences.
¡ Find information about different vendors online.
5. Design and Issue a Request for Information (RFI): Develop an RFI to solicit information from vendors
about their products and services. Ask for information about the vendor’s organizational prole,
implementation and training model, ongoing support, estimated total cost of ownership, and
availability for demonstrations. Be sure to include specic questions requesting documentation on
the vendor’s cybersecurity program including how they prepare for, mitigate against, and respond to
cybersecurity attacks.
3
Make it a requirement that any prospective MSP vendor set up ofine, off-
site, encrypted backups of information essential to your business.
4
6. Compare Vendors: Compare and evaluate RFIs returned by vendors. Rate the capabilities and the
vendor pricing to compare the costs of different MSPs. Using these comparisons will help you
narrow the eld further before conducting demonstrations.
7. Contact References and Schedule Site Visits: Ask vendors for lists of healthcare organizations who have
successfully implemented their managed service products. Contact the references and schedule
time to meet. Prepare a list of questions to gather lessons learned by the healthcare organization
before, during, and after implementation.
8. HIPAA Privacy Rule Requirements for Business Associate Agreements:
5
Business Associate Agreements
(BAAs) are a necessary tool for ensuring HIPAA Privacy Rule compliance. The negotiated terms of
BAAs are more important when a vendor will create or maintain patient information or the electronic
information systems that handle this data. Covered entities, such as physician practices and
healthcare facilities, are required to enter a BAA when they hire a third-party contractor to perform
a service on behalf of the covered entity (if the contractor will require the use of and/or access to the
1 “Gartner Peer Insights: Reviews Organized by Markets.” Gartner LLC. https://www.gartner.com/reviews/markets.
2 KLAS Research. https://klasresearch.com/.
3 “Cybersecurity for Small Business: Vendor Security.” Federal Trade Commission. https://www.ftc.gov/tips-advice/
business-center/small-businesses/cybersecurity/vendor-security.
4 Fair, Lesley. “Ransomware Risk: 2 Preventive Steps for Your Small Business.” Federal Trade Commission. November 5,
2021. https://www.ftc.gov/news-events/blogs/business-blog/2021/11/ransomware-risk-2-preventive-steps-your-
small-business.
5 “Business Associates.” HHS Ofce for Civil Rights. May 24, 2019. https://www.hhs.gov/hipaa/for-professionals/
privacy/guidance/business-associates/index.html.
Introduction
6Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
covered entity’s PHI to perform such service). Examples of potential third-party contractors include
outsourced IT management companies, EHR vendors, and cloud data storage services.
The Final Decision
After establishing managed IT service objectives and conducting a vendor assessment, select a vendor and
enter the contracting phase. For more information on vendor contracting, see What Are Important Items
to Include in a Vendor Contract? published by ONC for Health IT.
6
Managing Vendors to Protect Cybersecurity
The threat of a cybersecurity incident compromising patient data and causing disruption to treatment
activity still exists when outsourcing some/all the IT network management to an MSP vendor. As such,
small healthcare organizations should develop and implement a plan to manage and monitor an MSP
vendor’s cybersecurity risk. For example, vendors that host patient information or interface with medical
devices warrant more thorough monitoring cybersecurity practices compared to IT vendors who only
access the information system while performing services onsite.
Monitoring intensity should be based on the level of risk presented to the healthcare organization.
Monitoring can include requesting and reviewing security-related documentation from MSP vendors
such as cybersecurity policies, proof of training, proof of conducting background investigations on their
workforce members, third-party security evaluations, and risk assessments. If the vendor is hosting data
or systems, the documentation requested may be more specic (e.g., proof of backups, actual contingency
test reports, proof of terminations and destruction certicates). For an organization to remain informed
on its security posture, an Executive Business Review (EBR) on a periodic cycle (quarterly/bi-annually) can
be requested.
Monitoring to ensure vendors are compliant with industry best practices is especially signicant to avoid a
cybersecurity attack.
Finally, management of an MSP vendor’s activities does not cease on the termination date specied in
the service agreement or contract. Requirements detailing the disposition of both access and retention
of data should be included in the service agreement. The contract should also specify how to eliminate
and document all access to patient information, as well as instructions for returning or destroying all
patient information in MSP possession. This documentation is crucial should a breach occur involving
a healthcare organization’s information after that entity has terminated its relationship with the
MSP vendor.
As mentioned previously, the practices and recommendations in this volume are tailored to small
organizations. In some cases, small organizations could also benet from selected practices in Technical
Volume 2 of this publication, which focuses on medium and large organizations. However, size is not a
determinant of who might benet from the cybersecurity practices found in each volume.
6 “What Are Important Items to Include in a Vendor Contract?” Ofce of the National Coordinator for Health IT.
October 22, 2019. https://www.healthit.gov/faq/what-are-important-items-include-vendor-contract.
7Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
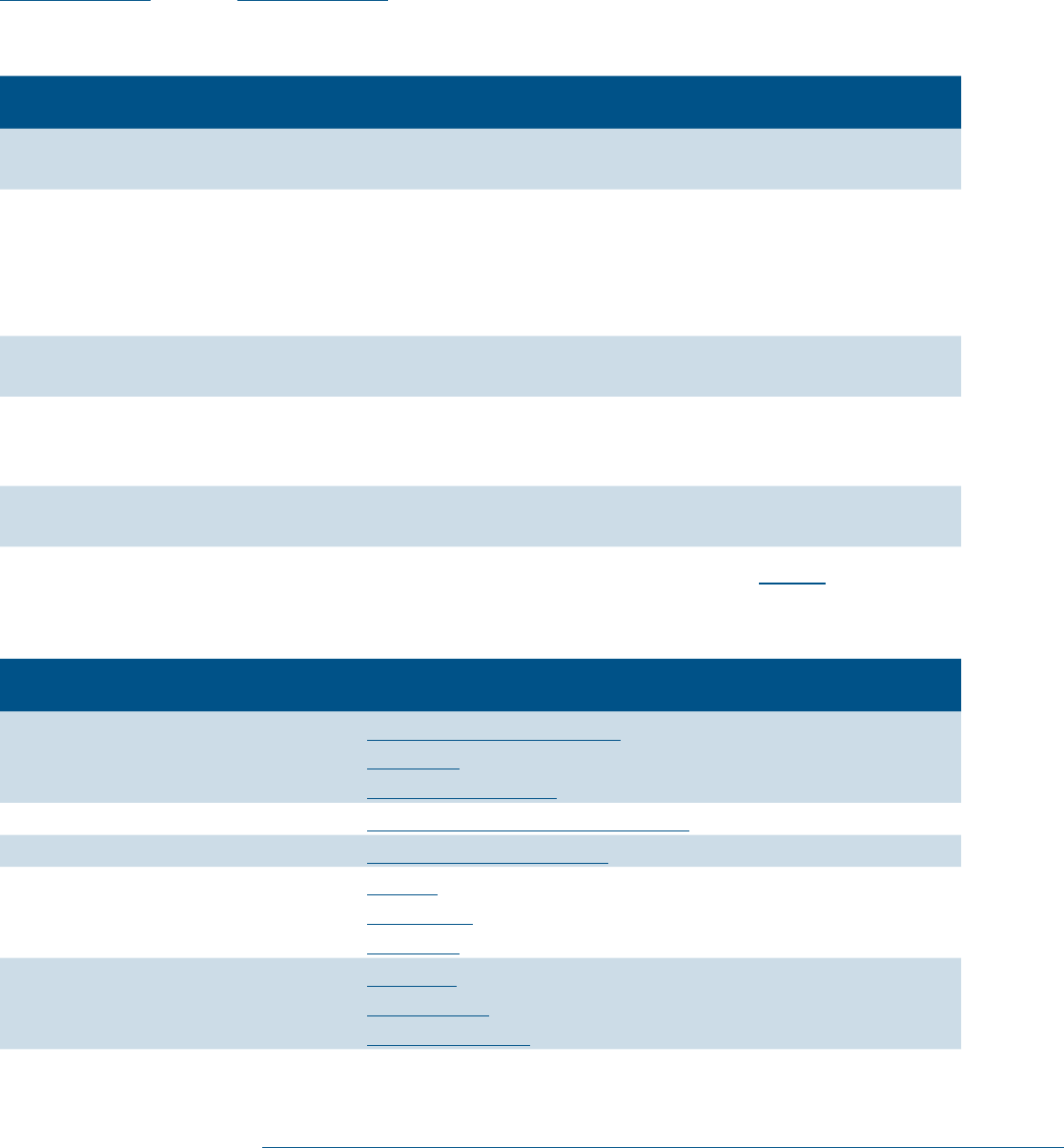
Document Guide: Cybersecurity Pracces
This volume provides small healthcare organizations with a series of cybersecurity practices to prevent,
react to, and recover from the ve cybersecurity threats identied below in Table 1 and discussed in the
Main Document. (See the Main Document for detailed denitions and descriptions of each threat.)
Table 1. Five Prevailing Cybersecurity Threats to Healthcare Organizations
Threat Potenal Impact of Aack
Social engineering Malware delivery or credential attacks. Both attacks further
compromise your organization.
Ransomware attack Information system assets locked and held for payment of ransom
(extortion). Disrupts normal healthcare operations. Prevents business
functions like electronic billing for treatment services. May result in a
breach of sensitive information and patient identity theft as well as the
permanent loss of patient records.
Loss or theft of
equipment or data
Breach of sensitive information. May lead to patient identity theft.
Insider, accidental or
malicious data loss
Removal of data from your organization (intentionally or
unintentionally). May lead to a breach of sensitive information as well
as patient identify theft.
Attacks against network
connected medical devices
Undermined patient safety, delay or disruption of treatment,
and well-being.
The cybersecurity practices and sub-practices to mitigate these threats are listed in Table 2 below.
Table 2. Cybersecurity Practices and Sub-Practices for Small Organizations
Cybersecurity Pracce Sub-Pracce for Small Organizaons
Email Protection Systems 1.S.A Email System Conguration
1.S.B Education
1.S.C Phishing Simulations
Endpoint Protection Systems
2.S.A Basic Endpoint Protection Controls
Access Management
3.S.A Basic Access Management
Data Protection and
Loss Prevention
4.S.A Policies
4.S.B Procedures
4.S.C Education
Asset Management
5.S.A Inventory
5.S.B Procurement
5.S.C Decommissioning

Document Guide: Cybersecurity Practices
8Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce Sub-Pracce for Small Organizaons
Network Management 6.S.A Network Segmentation
6.S.B Physical Security and Guest Access
6.S.C Intrusion Prevention
Vulnerability Management
7.S.A Vulnerability Management
Incident Response
8.S.A Incident Response
8.S.B Information Sharing
Network Connected Medical
Device Security
9.S.A Medical Device Security
Cybersecurity Oversight
and Governance
10.S.A Policies
10.S.B Cybersecurity Risk Assessment and Management
10.S.C Security Awareness and Training
10.S.D Cyber Insurance
9Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #1:
Email Protecon Systems
Most small practices leverage outsourced third-party email
providers, rather than establishing a dedicated internal email
infrastructure. This section’s email protection practices are
presented in three parts:
• Email system conguration: the components and capabilities that
should be included within your email system.
• Education: how to increase staff understanding and awareness
to protect your organization against email-based cyber-attacks
such as phishing and ransomware.
• Phishing simulations: ways to provide staff with training on and
awareness of phishing emails.
Small healthcare organizations should avoid “free” or “consumer”
email systems. These email offerings may not have safeguards
in place that meet the requirements of the HIPAA Security
Rule to store, process, or transmit PHI. Most widely available
internet service providers offer a level of service that will apply
the appropriate safeguards that meet HIPAA Security Rule
requirements. Ensure all vendors sign a BAA to meet HIPAA Security Rule requirements.
Sub-Practices for Small Organizations
1.S.A: Email System Conguration
NIST Framework Ref: PR.DS-2, PR.IP-1, PR.AC-7
Consider the following controls to enhance the security posture of your email system. Check with your
email service provider to ensure these controls are in place and enabled.
• Secure email for business use. Organizations should ensure that basic spam/antivirus software
solutions are installed, active, and automatically updated wherever possible. Many spam lters can
be congured to recognize and block suspicious emails before they reach employee inboxes.
7
Additionally, organizations that want a defensive strategy against malware attacks may want to
consider deployment of a “sinkhole”. This utilizes a server designed to capture malicious trafc and
prevent control of infected computers by the criminals who infected them. A Domain Name System
(DNS) sinkhole can act as a major tool for eradicating the spreading of malware infection risk areas
and can be used to break the command and control connection. There are many excellent free open
source tools that can be evaluated to determine the best one for your organization.
7 “Update Your Software Now.” Federal Trade Commission. June 2019. https://www.consumer.ftc.gov/blog/2019/06/
update-your-software-now.
Areas of Impact
Sensitive Data, System Integrity
Sub-Practices
1.S.A Email System
Conguration
1.S.B Education
1.S.C Phishing Simulations
Key Threats Addressed
• Social engineering
• Ransomware attacks
• Insider, accidental or
malicious data loss
405(d) Resources
• Prescription Poster:
Email Protection Systems
• Five Threats Flyers:
¡ Social Engineering
¡ Ransomware Attacks
¡ Insider, Accidental, or
Intentional Data Loss

Cybersecurity Pracce #1: Email Protecon Systems
10Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
• Deploy multi-factor authentication (MFA) before enabling access to your email system. MFA can prevent
hackers who have obtained a legitimate user’s credentials from accessing your system.
8
Make sure
that MFA is in place for web access and your local client access. It’s popular to want to use IMAP or
POP3 settings protocols, but these might not support MFA and can leave a back door open to your
email mailboxes.
• Optimize security settings within your authorized internet browser(s), including blocking specic websites
or types of websites. Optimization of security settings can minimize the likelihood than an employee
will open a malicious website link. Most browsers assess the possibility that a site is malicious and
send warning messages to users attempting to access potentially dangerous sites. The University
of California at Santa Cruz has developed a guide for security settings on several widely used
internet browsers.
9
• Congure your email system to tag messages that are sent from outside of your organization as
“EXTERNAL”. Consider implementing a tag that advises the user to be cautious when opening such
emails, for example, “Stop. Read. Think. This is an External Email.”
10
• Implement an email encryption service or module. This enables users to securely send emails to
external recipients or to protect information that should only be seen by authorized individuals.
• Provide every employee with a unique user account tied to a unique email address. These accounts and
email addresses should not be shared. Have a process in place to terminate user accounts when the
employee leaves your organization.
1.S.B: Education
NIST Framework Ref: PR.AT-1
Implement education and awareness activities to assist your employees and partners in protecting your
organization against phishing attacks. Common phishing attacks include email messages that attempt to
trick you into:
• divulging your usernames and passwords.
• downloading and installing software (this is the primary mechanism of installing malware
or ransomware).
• procuring gift cards or conducting wire transfers (also known as Business Email Compromise (BEC)).
To educate your users, it is important to distribute awareness materials and train your employees and
partners. Establish and maintain a training program for your workforce that includes a section on phishing
8 “Back to Basics: Multi-Factor Authentication.” NIST Information Technology Laboratory/Applied Cybersecurity
Division. February 16, 2022. https://www.nist.gov/itl/applied-cybersecurity/tig/back-basics-multi-factor-
authentication.
9 “Web Browser Secure Settings.” University of California Santa Cruz Information Technology Services. September 25,
2020. https://its.ucsc.edu/software/release/browser-secure.html.
10 Smith, Andrew. “Cybersecurity for Small Business: Email Authentication.” Federal Trade Commission. February
8, 2019. https://www.ftc.gov/news-events/blogs/business-blog/2019/02/cybersecurity-small-business-email-
authentication.
Cybersecurity Pracce #1: Email Protecon Systems
11Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
attacks.
11
All users in your organization should be able to recognize the phishing techniques outlined
below in Table 3.
12
Train your employees to do the following:
• Train your employees and partners to use the encryption module within your email system to minimize
the risk of information being intercepted by hackers.
• Train your employees to be careful when sending and receiving emails that contain personally
identiable information (PII) or PHI. When sending PII or PHI double check that the email address
of the intended recipient of the email message is correct so that the message is not received by the
wrong person.
13
• Train your employees how to report suspicious messages. These should be reported to the person
responsible for maintaining your IT system staff or contractor. That individual or service provider
can then advise the employee regarding disposition of the suspicious message. See Cybersecurity
Practice #8: Incident Response.
Table 3. Phishing Detection
Phishing Detecon Descripon
Check embedded links Validate that the URL of the link matches the text of the link itself. This
can be achieved by hovering (not clicking) your mouse cursor over the link
to view the URL of the website to be accessed. Always be careful when
clicking on an external link, as not all external links will direct you to a
trusted website.
Look for suspicious
“From:” addresses
Check received emails for spoofed or misspelled “From:” addresses.
For example, if your organization is “ACME” and you receive an email
from [email protected], do not open the email without verifying that it
is legitimate. You can check this by hovering over the sender’s name.
Legitimate addresses should match what is in the “From:” eld.
Be cautious with
“urgent” messages
If the email message requires immediate action, especially if it includes a
request to access your email or any other account, do not open the email or
take any action without verifying that it is legitimate.
Be cautious with “too
good to be true” messages
If you receive an unexpected message about winning money or gift
cards, do not open the email or take any action without verifying that it
is legitimate.
11 “Cybersecurity for Small Business: Phishing.” Federal Trade Commission. https://www.ftc.gov/tips-advice/business-
center/small-businesses/cybersecurity/phishing.
12 “How to Recognize and Avoid Phishing Scams.” Federal Trade Commission. May 2019. https://www.consumer.ftc.gov/
articles/how-recognize-and-avoid-phishing-scams.
13 “Security Tip ST04-014): Avoiding Social Engineering and Phishing Attacks.” Cybersecurity & Infrastructure Security
Agency (CISA). August 25, 2020. https://www.cisa.gov/news-events/news/avoiding-social-engineering-and-phishing-
attacks.
Cybersecurity Pracce #1: Email Protecon Systems
12Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
1.S.C: Phishing Simulations
NIST Framework Ref: PR.AT
An effective approach for training the workforce to detect a phishing attack is to conduct simulated
phishing and social engineering campaigns. The authorized cybersecurity personnel or third-party
provider crafts and sends phishing emails to users with email accounts. These emails have embedded
tracking components (e.g., to track link clicks). Tracking enables your organization to identify employees
who detect the email as a phishing attack and those who fail to detect the attack, opening the email or
clicking the emailed links. Your organization can then provide the appropriate training and feedback
as soon as possible after the event. Simulated phishing attacks provide a cause-and-effect training
opportunity and are incredibly effective. Consider conducting entire workforce phishing simulations on
at least a monthly basis. Develop specialized simulations for higher-risk areas within your organization.
These could be department-based (e.g., nance, human resources) or data-based e.g., highest-risk users).
Phishing and social engineering campaigns should track (and potentially reward) users that successfully
report the test message.
An effective phishing simulation should include:
• Implement regular (e.g., monthly, quarterly) campaigns with real-time training for your staff. Many
third-parties provide low cost, cloud-based phishing simulation tools to train and test your
workforce. These tools often include easy to distribute pre-congured training your workforce can
complete independently.
• Begin campaigns with easy-to-spot emails your workforce learns to recognize. Slowly increase the
sophistication of these simulations to improve the detection capability of your workforce. Also
consider sending email tests related to BEC, as discussed previously.
• Include targeted tests directed to leadership, accounts payable, payroll, and other workforce members
in positions that make them specic targets for phishing.
• Create special training and tests for workforce members who are frequently on the list of those who
clicked the link or opened an attachment.
CISA offers free phishing simulation services.
14
If you have budgetary limitations, it is advisable to contact
CISA and set up a service plan.
Although an anti-phishing campaign cannot stop the inbound ow of phishing emails, it will help your
organization identify any attacks that bypass established email security protections. Educated and aware
staff can become “human sensors” to inform you when a real phishing attack is occurring.
Key Mitigated Threats
1. Social engineering
2. Ransomware attack
3. Insider, accidental or malicious data loss
14 “Free Cybersecurity Services and Tools.” Cybersecurity & Infrastructure Security Agency (CISA). https://www.cisa.gov/
free-cybersecurity-services-and-tools.

13Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #2:
Endpoint Protecon Systems
Endpoints are IT devices and equipment that can provide access
to your organization’s information network.
15
Endpoints on an
organization’s information network include desktops, laptops,
mobile devices, and other connected hardware devices (e.g.,
printers, medical equipment). Because technology is highly mobile,
computers are often connected to and disconnected from an
organization’s network.
Although attacks against endpoints tend to be delivered via email,
as described above in Cybersecurity Practice #1: Email Protection
Systems, they can also be delivered as client-side attacks. Client-
side attacks occur when vulnerabilities within the endpoint are
exploited. Recommended security controls to protect endpoints are presented below in Table 4.
Sub-Practices for Small Organizations
2.S.A: Basic Endpoint Protection Controls
NIST Framework Ref: PR.AT, PR.IP-1, PR.AC-4, PR.IP-12, PR.DS-1, PR.DS-2, PR.AC-3
Table 4. Effective Security Controls to Protect Organization Endpoints
Security Control Description
Manage administrative
accounts
Administrative accounts are created and used by those authorized to make
changes to the information system. A separate administrative account
should be created for each person authorized to have privileges as a system
administrator and used for the installation of software. Only authorized
personnel within an organization should be allowed to install software
applications. The administrator of the system should not conduct their
non-administrative business tasks using their administrative account,
rather their “regular user account.”
Remove unnecessary
administrative accounts
Most users in an organization do not need to be authorized as system
administrators with expanded system access and capabilities. Remove
administrative access on endpoints to mitigate the damage that can be
caused by an attacker who compromises that endpoint.
15 Pahl, Thomas B. “Stick With Security: Secure Remote Access to Your Network.” FTC Bureau of Consumer Protection.
September 1, 2017. https://www.ftc.gov/ news-events/blogs/business-blog/2017/09/stick-security-secure-remote-
access-your-network.
Areas of Impact
Passwords, PHI
Sub-Practices
2.S.A Basic Endpoint
Protection Controls
Key Threats Addressed
• Ransomware attacks
• Loss or theft of equipment
or data
405(d) Resources
• Prescription
Poster: Endpoint
Protection Systems
Cybersecurity Pracce #2: Endpoint Protecon Systems
14Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Security Control Description
Audit your software
applications
Audit software applications on each endpoint. Maintain a list of approved
software applications. Remove unauthorized software applications as soon
as they are detected.
Always keep your
endpoints patched
Patching (i.e., regularly updating) systems removes vulnerabilities that
can be exploited by attackers. Each patch modies a software application,
mitigating a threat that has been exposed. Congure endpoints to patch
automatically and ensure third-party applications are patched as soon as
possible. It is often necessary to reboot or restart applications or system
software after applying updates or patches.
Implement antivirus
software
Antivirus software is readily available. For example, Microsoft Windows 10
operating system software has antivirus and malware security protections
pre-installed for the end-user to activate. Other vendors offer free or low-
cost software applications that are effective at protecting endpoints from
computer viruses, malware, spam, and ransomware threats. Each endpoint
in your organization should be equipped with antivirus software that is
congured to update automatically.
Remove End of Life (EOL)
operating systems
Remove End of Life (EOL) operating systems, software, and applications.
Operating systems, software, and applications are considered EOL when
they are no longer supported by the vendor/provider and do not receive
product updates and security patches. Use of these products represents
a signicant risk to your data, information systems, and overall mission.
Operating systems, software, and applications that are no longer supported
by the vendor/provider should be removed from the environment.
Enable endpoint
encryption
Install encryption software on every endpoint that can connect to your
information systems, especially mobile devices such as laptops. Maintain
audit trails of this encryption in the event a device is ever lost or stolen.
This simple and inexpensive precaution may prevent a complicated and
expensive breach. For devices that cannot be encrypted or that are
managed by a third-party, implement physical security controls to minimize
theft or unauthorized removal. Examples include installation of anti-theft
cables, locks on rooms where the devices are located, and the use of badge
readers to monitor access to rooms where devices are located.
Enable network rewalls Firewalls create a “buffer zone” between your own network and external
networks (such as the internet). Most popular operating systems now
include a rewall, so it may be as simple as switching this on. Enable
rewalls for your endpoint devices. Firewalls are especially important for
mobile devices that may be connected to unsecured networks such as Wi-
Fi networks at coffee shops or hotels.

Cybersecurity Pracce #2: Endpoint Protecon Systems
15Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Security Control Description
Enable MFA for
remote access
For devices that are accessed remotely, leverage technologies that require
MFA before permitting users to access data or applications on the device.
Logins that use only a username and password are no longer considered
truly secure due credentials often compromised through phishing emails.
If your healthcare organization uses an EHR or accesses sensitive data through a software application
(either on the cloud or onsite), encrypt network access to these applications. Contracts with EHR vendors
should include language that requires PHI to be encrypted both at rest and during transmission to and
from your systems. Software applications that encrypt data prevent hackers from accessing sensitive
data, usually by requiring a “key” to encrypt and/or decrypt data.
For healthcare organizations that have IT resources or contract with vendors to manage their information
systems, audit the use of remote access software that is installed on endpoints to ensure they remain in
use. Check to make sure that MFA is enabled on software applications and operating systems.
Finally, educate your workforce members on the need to report the loss or theft of endpoints to the
appropriate team or designated manager inside your organization. For example, if a backpack with a
laptop is stolen, the employee should report the theft promptly.
Key Mitigated Threats
1. Ransomware attack
2. Loss or theft of equipment or data
3. Attacks against devices that affect patient safety

16Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #3:
Access Management
Healthcare organizations of all sizes need to clearly identify all
users and maintain audit trails that monitor each user’s access to
data, applications, systems, and endpoints. Just as you may use a
name badge to identify yourself in the physical work environment,
cybersecurity access management practices can also help ensure
users are properly identied in the digital environment.
Sub-Practices for Small Organizations
User accounts enable organizations to control and monitor each
user’s access to and activities on devices, EHRs, email, and other
third-party software systems. It is essential to protect user accounts
to mitigate the risk of cyber threats. Your IT specialist should
implement the security controls outlined below in Table 5 to manage
user access of data, applications, and devices.
3.S.A: Basic Access Management
NIST Framework Ref: PR.AT, PR.AC-1, PR.AC-6, PR.AC-4, PR.IP-11, PR.IP-1, PR.AC-7
Table 5. Security Controls Enabling Organizations to Manage User Access to Data
Security Control Description
Establish a unique
account for each user
Assign a separate user account to each user in your organization. Train and
regularly remind users they are not to share passwords. Through policy
and awareness training, have each user create an account password that
is different from the ones used for personal internet or email access (e.g.,
Gmail, Yahoo, Facebook).
Limit the use of shared
or generic accounts
The use of shared or generic accounts should be avoided. If shared
accounts are required, train and regularly remind users that they must sign
out upon completion of activity or whenever they leave the device, even for
a moment.
Sharing accounts exposes organizations to greater vulnerabilities. For
example, the complexity of updating passwords for multiple users on a
shared account may result in a compromised password remaining active
and allowing unauthorized access over an extended period.
Areas of Impact
Passwords
Sub-Practices
3.S.A Basic Access
Management
Key Threats Addressed
• Ransomware attacks
• Insider, accidental or
malicious data loss
• Loss or theft of equipment
or data
• Attacks against network
connected medical
devices that may affect
patient safety
405(d) Resources
• Prescription Poster:
Identity and
Access Management
Cybersecurity Pracce #3: Access Management
17Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Security Control Description
Tailor access to the
needs of each user
Tailor access for each user based on the user’s specic workplace
requirements. Most users require access to common systems, such as
email and le servers. Implementing tailored access is usually called
‘role-based access’.
Terminate user access as
soon as the user leaves
your organization
When an employee or contractor ends their relationship with your
organization, ensure that procedures are in place to terminate their
information system access immediately. Prompt user termination prevents
former workforce members or contractors from accessing patient data
and other sensitive information after they have left your organization. This
is particularly crucial for organizations using cloud-based systems where
access is based on credentials, rather than physical presence at a particular
computer or device.
Any shared or generic accounts in use should also be updated.
User job duties change Similarly, if a workforce member or contractor changes roles within your
organization, it is important to terminate access related to their former
position. Be sure to terminate account settings for the prior role before
enabling a new set of permissions based on the requirements for the
new position.
Provide role-based access New user accounts must be granted user-appropriate access to your
organization’s information systems, computer workstations, and programs.
Allow each user access only to the computers, devices, and programs
required to accomplish that user’s job or role in your organization. This
limits your organization’s exposure to unauthorized access, loss, and theft
of data if the user’s identity or access is compromised.
Establish separate accounts for administrator roles segregated from
regular user access where a workplace member has responsibility as a
system administrator in addition to their system access as a regular user.
Enable MFA for all accounts that are created for administrators.
Periodic review of access Be sure to conduct a periodic review of all employees’ access to your in-
formation systems on a predetermined time frame.
Congure systems and
endpoints with automatic
lock and log-off
Congure systems, applications, and endpoints to automatically lock and
log-off users after a predetermined period of inactivity.
Implement single sign-on Implement single sign-on systems that automatically manage access to
all software and tools once users have signed onto the network. These
systems allow your organization to centrally maintain and monitor access.
Cybersecurity Pracce #3: Access Management
18Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Security Control Description
Use multi-factor
authentication
Require multi-factor authentication to access areas of your network with
sensitive information. This requires additional steps beyond logging in with
a password—like a push notication to an app installed on a smartphone,
temporary code delivered through short message service (SMS), or a key
that’s inserted into a computer.
Implement MFA for
VPN Access
Implement MFA for VPN connections used to connect to your
organization’s network and systems (whether those systems are located
on-premise or in the cloud).
Restrict use of elevated
privileged accounts
System administrators should be issued two accounts—one with elevated
privileges and another for routine ofce functions. The former should be
reserved for essential operations and limited access to email and any social
media platforms. This elevated privilege account name should be treated
as sensitive information and should not be disclosed outside of your
organization’s IT department.
Disable inbound Remote
Desktop Protocol (RDP)
Disable inbound Remote Desktop Protocol (RDP) on systems within your
organization’s network. Instead, set up a VPN tunnel for specic users and
systems that need to connect to your network remotely. Exploitation of
RDP is a common attack vector and considered a Bad Practice by CISA.
16
To monitor compliance with the practices listed in Table 5, implement access management procedures
to track and monitor user access to computers and programs. These procedures will promote consistent
provisioning and control of access throughout your organization. Examples of such standard operating
procedures can be found in the Cybersecurity Practices Assessments Toolkit.
Key Mitigated Threats
1. Ransomware attack
2. Insider, accidental or malicious data loss
3. Loss or theft of equipment or data
4. Attacks against network connected medical devices that may affect patient safety
16 “Bad Practices.” Cybersecurity & Infrastructure Security Agency (CISA). https://www.cisa.gov/BadPractices.
19Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #4: Data
Protecon and Loss Prevenon
A data security breach is the compromise, loss, or disclosure of
sensitive data, including information relevant to your organization’s
business and PHI. Impacts to your organization can be profound
if data is corrupted, lost, or stolen. Data security breaches may
prevent users from completing work accurately or on time and could
result in potentially devastating consequences to patient safety, the
provision of care and their well-being. Good data protection and
loss prevention practices protects an organization and its patients.
Sub-Practices for Small Organizations
The compromise of sensitive data can be prevented several
ways. Data protection is based on understanding where data
resides, where it is accessed, and how it is shared. Throughout this
document, there are many tips to protect data and prevent loss. This section focuses on loss prevention
policies, procedures, and education.
4.S.A: Policies
NIST Framework Ref: ID.GV-1, ID.AM-5
• Set the expectation on how your workforce is expected to manage the sensitive data at their ngertips.
Most healthcare employees work with sensitive data daily, so it is easy to forget how important it is
to remain vigilant about data protection. Organizational policies should address all user interactions
with sensitive data and reinforce the consequences of lost or compromised data.
• Establish a data classication policy that categorizes data by its criticality and sensitivity. Examples of
data classication are Sensitive, Internal Use, or Public Use. An organization needs to identify the
types of data les and types of records relevant to each category. For example, the Sensitive data
category should include PHI, social security numbers (SSNs), credit card numbers, which may be
used to commit fraud, or may damage your organization’s reputation. Table 6 outlines and describes
possible data classications.
• Prohibit the use of unencrypted storage media and devices, such as thumb drives, mobile phones, or
including computer hard drives. Require encryption of storage media before use.
Areas of Impact
Passwords, PHI
Sub-Practices
4.S.A Policies
4.S.B Procedures
4.S.C Education
Key Threats Addressed
• Ransomware attacks
• Insider, accidental or
malicious data loss
• Loss or theft of equipment
or data
405(d) Resources
• Prescription Poster:
Data Protection and
Loss Prevention

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
20Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Table 6. Example Data Classication Structure
Classication Description
Highly Sensitive PHI that can be used for identity theft, nancial fraud, or damage the
patient’s reputation. Examples include SSNs, credit card numbers,
behavioral health information, substance abuse information, and other
patient treatment information.
Data access should be controlled to only those users who need it to
perform their job or patient treatment as well as requiring proper
authentication at login. This data must be managed in compliance with
applicable regulatory requirements.
Sensitive Clinical research data, insurance information, human resources/employee
data, and business nancial records.
Internal Data that should be protected from public distribution. Examples
include organization policies and procedures, contracts, business
plans, corporate strategy and business development plans, and internal
business communications.
Public All data deidentied in compliance with applicable standards information
that is publicly available or otherwise permitted to be disclosed by
applicable federal or state requirements.
4.S.B: Procedures
NIST Framework Ref: ID.GV-1, PR.AT-1, PR.DS-2, PR.DS-5, PR.DS-1, PR.IP-6, ID.GV-3
Procedures to manage PHI ensure consistency through clear and explicit instructions. Such procedures
should therefore be implemented alongside data access policies. The following methods may be used to
develop and implement data management procedures:
• Use the classications dened in your policies to establish data usage procedures. For example,
Highly Sensitive data might have additional restrictions around disclosure than Sensitive data.
Identify authorized users of PHI and other Sensitive data. Establish the conditions for how and when
this data may be accessed or disclosed.
• Train your workforce to comply with organizational procedures when sending PHI via email.
Prioritize end-to-end encryption of PHI when sent via email or other messaging platforms. Patients
can request and receive PHI via unencrypted electronic communications. HHS has developed
materials to help educate patients that unencrypted communications containing PHI could be
accessed by a third-party in transit.
17
• Use an application that employs recognized secure email protocol and network for transmitting
PHI and other sensitive data via email. Implement data loss prevention technologies to mitigate
the risk of unauthorized disclosure of PHI and other Sensitive data. Refer to Technical Volume 2,
17 “FAQ 570: Does HIPAA permit health care providers to use e-mail to discuss with their patients?” HHS Ofce for
Civil Rights. July 26, 2013. https://www.hhs.gov/hipaa/for-professionals/faq/570/does-hipaa-permit-health-care-
providers-to-use-email-to-discuss-health-issues-with-patients/index.html.

Cybersecurity Pracce #4: Data Protecon and Loss Prevenon
21Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Practice #4: Data Protection and Prevention for details on the applicability of these
technologies to your organization.
• Train workforce members to avoid backing up data on storage devices that are not managed by your
organization or a user’s personal cloud service. For example, do not allow staff and physicians to
congure any workplace mobile device to back up to a personal computer unless that computer has
been congured to comply with your organization’s encryption and data security standards.
Note: Leveraging the cloud for backup purposes is acceptable if there are service and business
associate agreements in place with the vendor. Ensure compliance with agreements through
verifying the security of the vendor’s systems. Data being backed-up should be encrypted prior to
storage to a cloud vendor’s system.
• Apply appropriate safeguards to protect archived PHI to prevent unauthorized use or disclosure.
Audit and monitor access to this data to detect unauthorized use or disclosure.
• Ensure obsolete data are removed or destroyed properly once the retention period has elapsed.
Just as paper medical and nancial records must be fully destroyed by shredding or burning, digital
data must be properly disposed of to ensure that they cannot be inappropriately recovered. Discuss
options for properly disposing of outdated or unneeded data with your IT support. Do not assume
that deleting or erasing les means that the data are destroyed. See the Cybersecurity Practices
Assessments Toolkit for a sample data destruction form that can be used to ensure that data are
disposed of appropriately.
• Retain and maintain only data your organization requires to complete work or comply with records
storage requirements. Minimize your organization’s risk by regularly removing unnecessary data in
all your applications (as well as le folders of documents, spreadsheets, images, pdfs, etc.).
4.S.C: Education
NIST Framework Ref: PR.AT
Communicate the policies and procedures you implement to your staff. Make sure that all staff members
know how to classify and protect data as well as understand how the risks of data loss can affect
your organization.
• Provide educational and awareness materials to staff and physicians about organizational policies
implemented to safeguard information systems and data. At a minimum, provide annual and periodic
refresher training on the most salient policy considerations (e.g., the use of encryption and safe
transmission of PHI).
• Maintain a record of workforce training sessions, topics presented, and attendance.
Key Mitigated Threats
1. Ransomware attack
2. Loss or theft of equipment or data
3. Insider, accidental or malicious data loss

22Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #5:
Asset Management
Organizations manage IT assets using processes referred to
collectively as IT asset management (ITAM). ITAM is critical to ensure
appropriate cyber hygiene controls are maintained across all assets
in your organization.
ITAM processes should be implemented for all endpoints, servers,
networking equipment, and cloud applications. ITAM processes
enable organizations to understand their devices, and the best
options to secure them. The practices described in this section may
be used to support many of the practices described in other sections
of this volume. Although it can be difcult to implement and sustain
ITAM processes, such processes should be part of daily IT operations
and encompass the lifecycle of each IT asset, including procurement,
deployment, maintenance, and decommissioning (i.e., replacement
or disposal) of the device.
Sub-Practices for Small Organizations
5.S.A: Inventory
NIST Framework Ref: ID.AM-1
A complete and accurate ITAM leveraged by your organization facilitates the implementation of optimal
security controls. This inventory can be conducted and maintained using a well-designed spreadsheet.
The following information should be captured for each device:
• Asset ID (primary key)
• Host Name
• Purchase Order
• Operating System
• Media Access Control (MAC) Address
• IP Address
• Deployed To (User)
• User Last Logged On
• Purchase Date
• Cost
• Physical Location
Remember to include all devices owned and leveraged by your organization. This should include
workstations, laptops, servers, portable drives, mobile devices, tablets, printers, medical devices,
Areas of Impact
PHI
Sub-Practices
5.S.A Inventory
5.S.B Procurement
5.S.C Decommissioning
Key Threats Addressed
• Social engineering
• Insider, accidental or
malicious data loss
• Loss or theft of equipment
or data
• Attacks against network
connected medical
devices that may affect
patient safety
405(d) Resources
• Prescription Poster:
IT Asset Management
Cybersecurity Pracce #5: Asset Management
23Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
routers, access points, rewalls, software applications, and smart phones. Refer to Technical Volume 2,
Cybersecurity Practice #5: IT Asset Management for more information on how to construct and maintain
an effective inventory of IT assets.
5.S.B: Procurement
NIST Framework Ref: ID.AM-6
Upon creating the ITAM system, it is important to record each new IT asset as it is acquired. This requires
establishing standard operating procedures for procurement. Generally, it is advisable to assign the
responsibility of collecting information on new assets to the purchaser within your organization.
As an asset is acquired, it is critical to tag it with an asset tag. These tags can be physical or logical. The
tagging process ensures that the asset has a unique ID that can be used to identify it in the ITAM system.
Using existing data (e.g., hostname, IP address, MAC address) as the unique ID is not recommended,
because these elds may change, potentially creating duplicate records.
5.S.C: Decommissioning
NIST Framework Ref: PR.IP-6, PR.DS-3
IT assets no longer in use should be decommissioned in accordance with your organization’s procedures.
Small organizations should consider working with an outside service provider specializing in secure
destruction of IT hardware assets and data stored on media. Such providers can ensure that all data,
especially Sensitive data, are properly and securely destroyed from a device before it is placed into the
waste stream or turned over to other parties.
Additionally, your standard operating procedures should require you to record the decommissioning of
each device. If you use a service provider to decommission or destroy devices, record the certication of
destruction so there is documentation memorializing the process for destruction.
Key Mitigated Threats
1. Ransomware attack
2. Loss or theft of equipment or data
3. Insider, accidental or malicious data loss
4. Attacks against network connected medical devices that may affect patient safety
24Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #6:
Network Management
Networks—two or more computers or other digital devices that
are congured to share data—may be connected wirelessly or
via wired connections (e.g., network cables). Networks must be
established before systems can exchange information. Networks
established without cybersecurity controls or safeguards increase
an organization’s exposure to cyber-attack.
For this reason, networked devices must be managed so that they
exchange data safely and securely. When network management
is provided by a third-party IT support vendor, the healthcare
organization’s IT leaders must understand key aspects of proper
network management. Healthcare organizations must have
processes to ensure that effective network management practices
are included in contracts for these services.
Sub-Practices for Small Organizations
6.S.A: Network Segmentation
NIST Framework Ref: PR.AC-5, PR.AC-3, PR.AC-4, PR.PT-3
Congure networks to restrict access between devices, limiting data exchange to only what is required
to successfully execute operations. This reduces the risk of cyber-attacks from spreading across
your network.
18
• Restrict all internet-sourced access from computers and other digital devices into your organization’s
network. If your host servers are accessible directly from the internet, consider using a third-party
vendor to provide security as part of a hosting service.
• Restrict access to assets with potentially high impact in the event of compromise by placing them in more
restricted network zones. This includes medical devices and IoT items (e.g., security cameras, badge
readers, temperature sensors, building management systems).
• Only allow third parties, including vendors, access to networks that are necessary to their role or
responsibility. Allow them to connect only through tightly controlled interfaces. This limits the
exposure and impact of cyber-attacks on your organization as well as on the third-party vendor.
• Establish and enforce network trafc restrictions. These restrictions may apply to applications and
websites. Restricting network connections to personal websites (e.g., social media, couponing, online
shopping) limits exposure to browser add-ons or extensions, reducing the risk of cyber-attacks.
18 “Start with Security: A Guide for Business.” Federal Trade Commission. June 2015. https://www.ftc.gov/tips-advice/
business-center/guidance/start-security-guide-business#Remote.
Areas of Impact
PHI
Sub-Practices
6.S.A Network Segmentation
6.S.B Physical Security and
Guest Access
6.S.C Intrusion Prevention
Key Threats Addressed
• Ransomware attacks
• Loss or theft of equipment
• Insider, accidental or
malicious data loss
• Attacks against medical
devices that can affect
patient safety
405(d) Resources
• Prescription Poster:
Network Management

Cybersecurity Pracce #6: Network Management
25Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
6.S.B: Physical Security and Guest Access
NIST Framework Ref: PR.AC-4, PR.AC-2, PR.PT-3, PR.AC-5
Just as network devices need to be secured, physical access to the server and network equipment should
be restricted. Congure physical spaces and wireless networks to only allow permitted access.
• Always keep data and network closets locked. Grant access using badge readers or door locks with
coded access rather than traditional key locks. For brass locks or shared coded door locks, consider a
means to audit access, such as a security camera with continuous recording. Change the combination
periodically as well as after the departure of any former employees who knew the code.
• Disable network ports not in use. Maintain network ports as inactive until an activation request is
authorized. This minimizes the risk of an unauthorized user accessing your network by “plugging in”
to an empty port.
• Establish guest networks that separate organizational data and systems. For example, use guest
networks in conference rooms or waiting areas to provide separation and limit access to sensitive or
privileged data from guests (or others who have not been authorized to have system access). Ensure
guest networks are congured to access authorized guest services only.
6.S.C: Intrusion Prevention
NIST Framework Ref: PR.IP-1
Implement intrusion prevention systems as part of your network protection plan. This provides ongoing
protection to your organization’s network. Most modern rewall technologies used to segment your
network include an intrusion prevention systems (IPS) component. Implementing IPS and conguring
automatic updates reduces your organization’s vulnerability to known types of cyber-attacks.
IPS are available as part of a suite of next-generation network applications or as stand-alone products that
can be added to existing networks.
The recommendations in this sub-practice may necessitate a level of expertise to implement, requiring the
assistance of a qualied third-party support service to implement and manage these controls.
Key Mitigated Threats
1. Ransomware attack
2. Loss or theft of equipment or data
3. Insider, accidental or malcious data loss
4. Attacks against medical device that may affect patient safety
26Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #7:
Vulnerability Management
Vulnerability management is the process used by organizations to
detect technology aws that hackers could exploit. This process
uses a scanning capability, often provided by an EHR or IT support
vendor, to proactively scan devices and systems in your organization.
Sub-Practices for Small Organizations
7.S.A: Vulnerability Management
NIST Framework Ref: PR.IP-12
As discussed in the introduction to this volume, weak passwords,
default passwords, outdated software, and other technology
aws identied by vulnerability management scans are commonly
referred to as vulnerabilities. Vulnerability scans may yield large amounts of data, which organizations
urgently need to classify, evaluate, and prioritize to remediate security aws before an attacker can
exploit them. Vulnerability scanning can be conducted as an unauthenticated scan (without credentials)
or an authenticated scan (with credentials). Unauthenticated scans might produce more false
positives whereas authenticated scans will likely detect more vulnerabilities. It is recommended to use
authenticated scanning where you can.
To include vulnerability management practices in your organization:
• Schedule and conduct vulnerability scans on servers and systems under your control to proactively
identify technology aws.
• Remediate aws based on the severity of the identied vulnerability. Assign an owner to the
vulnerabilities that are discovered and track their remediation progress.
• Institute and implement regular processes to conduct web application scanning of internet-facing
webservers, such as web-based patient portals. Specialized vulnerability scanners can interrogate
running web applications to identify vulnerabilities in the application design.
• Establish policies and procedures to conduct routine patching of security aws in servers,
applications (including web applications), and third-party software. Maintain software at least
monthly, implementing patches distributed by the vendor community, if patching is not automatic.
Robust patch management processes, as outlined in 2.S.A: Basic Endpoint Protection Controls,
mitigate vulnerabilities associated with obsolete software versions, which are often easier for
hackers to exploit.
Key Mitigated Threats
1. Ransomware attack
2. Insider, accidental or malicious data loss
3. Attacks against network connected medical devices that may affect patient safety
Areas of Impact
PHI
Sub-Practices
7.S.A Vulnerability
Management
Key Threats Addressed
• Ransomware attacks
• Insider, accidental or
malicious data loss
• Attacks against network
connected medical
devices that can affect
patient safety
405(d) Resources
• Prescription Poster:
Vulnerability Management
27Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce
#8: Incident Response
Incident response (IR) is the ability to discover cyber-attacks on the
network and prevent them from causing further damage within
the network. IR is often referred to as the standard “blocking and
tackling” of cybersecurity.
Many types of security incidents occur on a regular basis across
organizations of all sizes. Two common security incidents that affect
organizations of all sizes are 1) the installation and detection of
malware, and 2) phishing attacks including malicious payloads (via
attachments and links). These incidents can enable a breach or loss
to occur through subsequent events.
Sub-Practices for Small Organizations
8.S.A: Incident Response
NIST Framework Ref: PR.IP-9
IR management is often a challenge for small healthcare organizations, in part because procedures may
not be established, or preparations have not been made. Employees who rarely encounter cyber-attacks
or other cybersecurity incidents may not remember what to do when a system is compromised. Without
well-planned and practiced IR processes, members of the management team may not know whom to
contact to obtain or provide information about the cyber-attack. In many cases, there are no dedicated
cybersecurity professionals in small organizations, resulting in increased reliance on the IT department
or vendors.
An Incident Response Plan (IRP) outlines the procedures to be followed after a cybersecurity incident,
including a cyber-attack. Without an IRP, the process of managing cybersecurity incident security breach
damage becomes cumbersome and confusing. This leads to an unnecessary waste of time and money,
disrupts the provision of patient care, and could affect patient safety.
What’s an Incident Response Plan in Actual Terms?
An IRP can be dened as a set of instructions offering a structured approach to detect, resolve, and
restore the damage sustained after a cybersecurity incident. An IRP also identies and species the roles
and responsibilities of the IR team at the time of the cyber-attack, examples of these types of attacks
can be found below in Table 7. The Computer Security Incident Response team (CSIRT) ensures that the
breach can be counteracted as per the IRP in the least possible time and with more efciency to keep the
damage, disruption to patient care and cost of recovery to a minimum.
19
19 Bartock, Michael et al. “NIST Special Publication 800-184: Guide for Cybersecurity Event Recovery.” National
Institutes of Standards and Technology (NIST). December 2016. https://nvlpubs.nist.gov/nistpubs/SpecialPublications/
NIST.SP.800-184.pdf.
Areas of Impact
PHI
Sub-Practices
8.S.A Incident Response
8.S.B Information Sharing
Key Threats Addressed
• Social engineering
• Ransomware attacks
• Loss or theft of equipment
or data
• Insider, accidental or
malicious data loss
• Attacks against network
connected medical
devices that can affect
patient safety
405(d) Resources
• Prescription Poster:
Incident Response
Cybersecurity Pracce #8: Incident Response
28Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Recognizing that small healthcare organizations encompass a broad range of capabilities and resources,
organizations should consider how best to develop contingencies that align with their capacity to support
the development and execution for IR planning.
20
Table 7. Roles and Responsibilities of an Incident Response Team
Role Responsibilities
Incident Commander Individual who oversees the cybersecurity incident and interacts with other
IR team stakeholders.
Executive/
Senior Leadership
An organization’s C-suite or most senior executives. They provide overall
direction and approvals required to resolve signicant cybersecurity
breaches. These individuals should be kept informed throughout the
lifecycle of a signicant cybersecurity incident.
Cybersecurity Teams Teams comprised of people with cybersecurity expertise who understand
attacks, vulnerabilities, and the methods by which threat vectors are
exploited. They provide technical knowledge and detail to technical teams
and execute procedures in the playbook.
Technical Teams Teams comprised of SMEs for the technologies that have been compromised
and who are engaged in developing and implementing the response. These
SMEs may be system owners, system administrators, or other individuals
with specialized IT expertise. They take instruction from the cybersecurity
teams as part of the playbook execution.
Legal Teams Teams comprised of attorneys in your general counsel (internal or external)
that help manage the incident under privilege as well as consult on
regulatory expectations.
Emergency Management With the potential for cybersecurity incidents to have an operational and
patient safety impact, a clinical emergency management function should
be connected to the CSIRT. In some organizations the CSIRT may take
direction from emergency management, in others it may be reversed. This
relationship should be determined prior to an incident.
Public Affairs/Marketing
and Communications
People who manage external and internal communications to deliver a
consistent voice and message in the event of a high-visibility cybersecurity
incident. This team is crucial in proactively managing the reputation of
your organization.
Privacy and
Compliance Team
Teams responsible for understanding the full extent of a cybersecurity
incident that involves PII/PHI. This includes conducting a breach assessment
for compliance with federal/state reporting and notication requirements.
20 Toth, Patricia. “Recovering from a Cybersecurity Incident: What to do Before and After.” NIST. https://www.nist.gov/
document/recovery-webinarpdf.
“Data Breach Response: A Guide for Business.” Federal Trade Commission (FTC). February 2021. https://www.ftc.gov/
tips-advice/business-center/guidance/data-breach-response-guide-business.

Cybersecurity Pracce #8: Incident Response
29Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Role Responsibilities
Other external teams Supporting an incident may require specialized forensics teams, law
enforcement, representatives from CISA or the Health Sector Cybersecurity
Coordination Center (HC3), and other teams to support the investigation
and remediation of the incident.
For more details and templates, visit CISA’s Cyber Incident Response page. CISA also offers Tabletop
Exercise Packages your organization can use to practice responding to a cyber incident and to test the
effectiveness of your IRP.
For further details on how to conduct incident response activities, refer to Technical Volume 2, Practice 8:
Security Operations and Incident Response.
8.S.B: Information Sharing
NIST Framework Ref: ID.RA-2
Establish a method to receive notications about cyber threats that are actively targeting other
organizations. The most effective way to do this is to join an information sharing and analysis organization
(ISAO) or information sharing and analysis center (ISAC). Participating in an appropriate ISAO or ISAC
is a great way to manage IR. Example ISACs used within the Healthcare Industry are the H-ISAC and the
Population Health ISAC (PH-ISAC).
21
Another resource is the Health Sector Cybersecurity Coordination Center (HC3) operated by the
Department of Health and Human Services. HC3 was created to aid in the protection of vital, healthcare-
related, controlled information and ensure cybersecurity information sharing is coordinated across the
Health and Public Health Sector (HPH).
22
Among the products of value to small healthcare organizations
are sector alerts to provide insight into cybersecurity threats and vulnerabilities. To subscribe to HC3’s
sector alerts, email [email protected].
Lastly, a review of the services provided by the DHS CISA is recommended. CISA provides a series of free
cybersecurity services and tools, including feeds of known Indicators of Compromise (IOCs) that can be
congured to be automatically blocked at your rewall and endpoints.
23
Key Mitigated Threats
1. Social engineering
2. Ransomware attack
3. Loss or theft of equipment or data
4. Insider, accidental or malicious data loss
5. Attacks against network connected medical devices that may affect patient safety
21 Health-ISAC. https://h-isac.org/.
“CommHIT Information Sharing & Analysis Centers.” CommunityHealth IT. https://www.communityhealthit.org/isacs/.
22 “Health Sector Cybersecurity Coordination Center (HC3).” U.S. Department of Health and Human Services (HHS).
March 31, 2022. https://www.hhs.gov/about/agencies/asa/ocio/hc3/index.html.
23 “Free Cybersecurity Services and Tools.” Cybersecurity and Infrastructure Security Agency (CISA). https://www.cisa.
gov/free-cybersecurity-services-and-tools.

30Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #9:
Network Connected Medical
Devices
Medical devices are ubiquitous in small healthcare organizations.
They are essential tools for providing diagnostic, therapeutic and
treatment services. Medical devices deliver signicant benets and
are successful in the treatment therapies.
As technology advances and healthcare environments migrate to
digitized systems, so do the complexity and sophistication of medical
devices. For many reasons, it is highly desirable to interface medical
devices directly with clinical systems. Automating data collection
from medical devices reduces the labor burden and exposure
to human error that results from manual input of data. For example, bedside vital signs monitors are
networked to centralized nursing station displays and alarms. Infusion pumps are networked to servers to
distribute drug libraries as well as download usage data.
As with all technologies, medical device benets are accompanied by cybersecurity challenges. An
emerging threat is the hacking of medical devices which can jeopardize patient safety by operations in an
unintended manner. For example, the 2015 video “How to Hack an Infusion Pump”
24
demonstrates how
an infusion pump can be controlled remotely to modify the dosage of drugs, threatening patient safety.
Cybersecurity vulnerabilities are introduced when medical devices are connected to a network or
computer to process required updates. Many medical devices are managed remotely by third-party
vendors, which further increases the attack footprint.
Sub-Practices for Small Organizations
9.S.A: Medical Device Security
NIST Framework Ref: PR.PT
If your organization connects medical devices to a network, consider the practices recommended in
Technical Volume 2, Cybersecurity Practice #9: Network Connected Medical Devices.
Key Mitigated Threats
1. Attacks against network connected medical devices that may affect patient safety
24 Versel, Neil. “How easy is it to hack an infusion pump? Watch this video.” MedCity News. August 10, 2015. https://
medcitynews.com/2015/08/hack-infusion-pump-video/.
Areas of Impact
PHI
Sub-Practices
9.S.A Medical Device Security
Key Threats Addressed
• Attacks against network
connected medical
devices that can affect
patient safety
405(d) Resources
• Prescription Poster:
Network Connected
Medical Devices
31Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Cybersecurity Pracce #10:
Cybersecurity Oversight
and Governance
Owners and executives of small healthcare organizations have
limited time and resources to devote to the oversight, development,
implementation, and monitoring of a comprehensive cybersecurity
risk management program. While cybersecurity risk management
practices are typically beyond the expertise of owners and
executives of small healthcare organizations, the increased focus by
regulators and the public requires those owners and executives to
be aware of key oversight and governance responsibilities. Given
limited time and resources, the intent is to identify reasonable
sub-practices that allow small healthcare organization owners and executives to establish a culture
of cybersecurity and properly manage risk (without taking away the ability to implement the nine
cybersecurity practices previously outlined).
Sub-Practices for Small Organizations
10.S.A: Policies
NIST Framework Ref: IG.GV-1, ID.AM-6, PR.AT, PR.AT-1, RS.CO
Policies are rst established, then supplemented with procedures to implement the policies. Policies
describe what is expected, and procedures describe how the expectations are met.
For example, a policy is established that all users will complete privacy and security training. The policy
species that training courses will be developed and maintained for both privacy and security, that all
users will complete the training, that a particular method will be used to conduct the training, and that
specic actions will be taken to address noncompliance with the policy. The policy does not describe how
your workforce will complete the training, nor does it identify who will develop the courses. Procedures
provide these details, for example, by clearly stating that privacy and security professionals will develop
and release the courses. Additionally, the procedures describe the process to access the training.
Written policies and procedures are important tools to ensure the security safeguards you decide to
implement are done so consistently. If workforce members are trained and have a reference manual
to conrm they are following the proper steps required to maintain security, they will be much
more successful.
Example of a self-assessment toolkit is provided in the Cybersecurity Practices Assessments Toolkit.
Policy examples with descriptions and recommended users are provided below in Table 8.
Areas of Impact
N/A
Sub-Practices
10.S.A Policies
10.S.B Cybersecurity Risk
Assessment and
Management
10.S.C Security Awareness and
Training
10.S.D Cyber Insurance
405(d) Resources
• Prescription Poster:
Cybersecurity Policies
Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
32Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Table 8. Effective Policies to Mitigate the Risk of Cyber-Attacks
Policy Name Descripon User Base
Roles and Responsibilities Describe cybersecurity roles and
responsibilities throughout your
organization, including who is responsible for
implementing security practices and setting
and establishing policy.
• All users
Education and Awareness Describe the mechanisms by which the
workforce will be trained on cybersecurity
practices, threats, and mitigations.
• All users
• Cybersecurity team
Acceptable Use/Email Use Describe what actions users are permitted
and not permitted to execute, including
detailed descriptions of how email will be
used to complete work.
• All users
Data Classication
Describe how data will be classied, with
usage parameters for each classication.
This classication should be in line with
Cybersecurity Practice #4: Data Protection
and Loss Prevention.
• All users
Personal Devices Describe your organization’s position on
usage of personal devices, also referred
to as bring your own device. If usage of
personal devices is permitted, describe
the expectations for how the devices will
be managed.
• All users
Laptop, Portable Device,
and Remote Use
Describe the policies that relate to mobile
device security and how these devices may
be used in a remote setting.
• All users
• IT Team
Incident Reporting
and Checklist
Describe requirements for users to report
suspicious activities in your organization
and for the cybersecurity department to
manage IR.
• All users
• Cybersecurity team

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
33Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
10.S.B: Cybersecurity Risk Assessment and Management
NIST Framework Ref: ID.RA
A cybersecurity risk assessment (RA) helps your organization measure the likelihood of known threats
and vulnerabilities compromising data and information assets. This allows for identifying any gaps
in cybersecurity safeguards and controls that are in place and determines if it reduces the risk to an
acceptable level. An RA is an important step in both protecting your workers and your organization and
complying with the HIPAA Security Rule. It helps you focus on the risks that really matter and prepare
for what could go wrong. An RA can help your organization understand potential risks and prioritize the
risks that need to be fully addressed. This should not be done in a silo but should be an organizational
collaborative effort.
Managing the security risks associated with the healthcare industry’s growing reliance on IT is a
continuous challenge. HIPAA Security Rule, CMS’ Promoting Interoperability Program (formerly
known as Meaningful Use), and several state’s data protection requirements for PHI require healthcare
organizations to conduct formal RAs.
There are various frameworks available when conducting an RA. The HHS OCR has provided guidance
on how to conduct a risk assessment.
25
In addition to conducting the RA, it is advised to align your
cybersecurity program to the NIST Cybersecurity Framework.
26
The key to an effective RA is to identify all information technology assets across your organization
that handles PHI; and, to ensure the scope of the RA captures the threats or vulnerabilities that could
jeopardize the condentiality, integrity and availability of PHI. To do this, be sure to:
• Document the threats and vulnerabilities within the information system.
• Evaluate the potential impact and the effectiveness of existing safeguards and controls.
• Determine the likelihood of occurrence that the threat or vulnerability could compromise data or
information system assets.
It is important to remember that performing an RA is an ongoing process, in which an organization:
• Regularly reviews its records to track access to PHI and detect security incidents.
• Periodically evaluates the effectiveness of current security measures.
• Regularly evaluates the vulnerabilities and threats to PHI.
Healthcare organizations have struggled to nd efcient ways to ensure cybersecurity threats, driven
by human action, mother nature or technology aw, affecting their operations are fully addressed with
appropriate controls to mitigate the risks. Enterprise Risk Management (ERM)
27
can help identify,
communicate, and categorize an organization’s top risk areas.
Some RA considerations for cybersecurity and privacy leaders:
25 “Guidance on Risk Analysis.” HHS Ofce of Civil Rights (OCR). Last reviewed July 22, 2019. https://www.hhs.gov/
hipaa/for-professionals/security/guidance/guidance-risk-analysis/index.html.
26 “Small Business Cybersecurity Corner: NIST Cybersecurity Framework.” NIST. Last reviewed April 14, 2022. https://
www.nist.gov/itl/smallbusinesscyber/planning-guides/nist-cybersecurity-framework.
27 Enterprise Risk Management is an effective organization-wide approach to addressing the full spectrum of your
organization’s signicant risks by understanding the combined impact of risks as an interrelated portfolio rather than
addressing risks only within silos.” See “Circular No. A-11.” Executive Ofce of the President Ofce of Management
and Budget (OMB). Section 260. August 2022. https://www.whitehouse.gov/wp-content/uploads/2018/06/a11.pdf.

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
34Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
• An RA should be the rst requirement in any security program or framework. It informs and
measures how well controls are working to mitigate risk and reduce liability. Not having an effective
RA is like not having a foundation to your home. Without a risk assessment, you are making decisions
based on an incomplete picture. In addition, both HIPAA Security Rule, and in some cases, state law
requires cybersecurity management. The risk assessment is a good starting point to meeting your
regulatory requirements.
• An organization’s leadership team plays a central role in ensuring resources are properly allocated to
the most vulnerable areas of your organization. Proactive risk management will preserve and protect
your organization’s nancial viability and human assets. Risk management processes should be put in
place to protect your organization’s limited budget and resources.
Correctly and periodically conducting a risk assessment is critical to building and maintaining an informed
risk management program, and ultimately, a robust cybersecurity program. Done well, it can reap many
benets from saving dollars, to avoiding compliance issues, and mitigating potential causes of disruption.
Simply put, it helps protect your business, your investment, and most importantly, your patients.
The HIPAA Security Rule requires that covered entities and its business associates conduct a risk
assessment of their healthcare organization. The ONC, in collaboration with the HHS OCR, developed
a downloadable Security Risk Assessment (SRA) Tool to help guide you through the process.
28
The tool
is designed to help healthcare providers conduct a security risk assessment as required by the HIPAA
Security Rule and the CMS EHR Incentive Program. The target audience of this tool is medium and small
providers; thus, use of this tool may not be appropriate for larger organizations. The HICP publication has
also been featured in this tool.
The NIST Small Business Cybersecurity Corner also provides a wealth of guides, resources, and case
studies to protect information and reduce cybersecurity risk.
29
28 “Security Risk Assessment Tool.” Ofce of the National Coordinator for HealthIT. Last modied February 15, 2022.
https://www.healthit.gov/topic/privacy-security-and-hipaa/security-risk-assessment-tool.
29 “Small Business Cybersecurity Corner: NIST Cybersecurity Framework.” National Institutes of Science and Technology
(NIST). Last modied April 14, 2022. https://www.nist.gov/itl/smallbusinesscyber/planning-guides/nist-cybersecurity-
framework.
Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
35Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
10.S.C: Security Awareness and Training
NIST Framework Ref: PR.AT
Train personnel to comply with organizational policies. At minimum, provide annual training on the most
salient policy considerations, such as the use of encryption and PHI transmission restrictions.
Studies show that most successful email and ransomware attacks are caused by human error. As such,
Security Awareness Training (SAT) is a critical component of every cybersecurity plan. Designate
responsibility for implementation and monitoring to document effectiveness. Real-time learning is
proven as highly effective and should include full and part-time employees and all levels of management.
Persons with access to information systems from outside the company, including contractors and vendors,
may also require training.
An example of SAT is outlined in Cybersecurity Practice #1: Email Protection Systems. Training should
begin during the on-boarding process. An initial test to benchmark the failure rate will enable progress to
be tracked and identify employees, and others with access to the information system, who may need extra
attention to be successfully trained. Avoid sending the same email to employees who work together, as
they may share information and cause inaccurate results.
While SAT programs primarily focus on phishing emails, entities could attempt to integrate this strategy
as part of a broader scope of training to fulll the standards of the HIPAA Privacy and Security Rules or
similar state data protection laws. Policies concerning key security topics may be developed and included
in the SAT program. Suggested topics with examples:
• Facility security, such as caution with visitors to avoid access to sensitive information.
• Workstation security, which could include protecting screens from unauthorized viewing and a “clean
desk” policy.
• Security policy training, such as policies restricting use of external drives and keeping
passwords secure.
The HHS 405(d) program has developed a one page document titled How to Implement Cybersecurity
Workforce Training for Small Healthcare Organizations your organization can use to develop its
SAT program.
30
10.S.D: Cyber Insurance
NIST Framework Ref: ID.RM, ID.GV
Cyber insurance is one option that can help protect your business against losses resulting from a cyber-
attack. If you are thinking about cyber insurance, discuss which policy would best t your company’s
needs with your insurance agent. This should include whether you should go with rst-party coverage,
third-party coverage, or both.
31
Be advised that many policies require you have a minimum level of
security controls in place. You should not secure a cyber insurance policy in lieu of implementing the
cybersecurity practices outlined in this document.
30 How to Implement Cybersecurity Workforce Training: Cybersecurity Workforce Training for Small Healthcare Organizations.
HHS 405(d) program. https://405d.hhs.gov/Documents/405d-howto-cyberworkforcetraining-small.pdf.
31 “Cybersecurity for Small Business: Cyber Insurance.” Federal Trade Commission (FTC). https://www.ftc.gov/tips-
advice/business-center/small-businesses/cybersecurity/cyber-insurance.

Cybersecurity Pracce #10: Cybersecurity Oversight and Governance
36Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
What Should Your Cyber Insurance Policy Cover?
Be sure your policy includes coverage for:
• Data breaches (like incidents involving theft of personal information)
• Cyber-attacks on your data held by vendors and other third parties.
• Cyber-attacks (breaches of your network)
• Cyber-attacks that occur anywhere in the world (not just in the United States)
• Cyber-attacks determined to be nation-state attackers
• Cyber-attacks aided by insiders both intentional and unintentional
• Cyber-attacks that lead to extortion (ransomware attacks)
• Terrorist acts
• Cyber warfare
Also, consider whether your cyber insurance provider will:
• Defend you in a lawsuit or regulatory investigation (called a “duty to defend”)
• Provide coverage more than any other applicable insurance you have
• Offer a breach hotline that’s available every day of the year at-all-times
• Provide access to third-party breach specialists, including forensics, independent legal counsel
working on your behalf, not the cyber insurance provider, and incident remediation rms
• Require you to use specic vendors for IR
• Provide coverage for notication costs including printing, mailing, phone centers, and PR assistance
• Loss of business coverage or revenue
Review your application closely and answer any questions about your business to the best of your ability.
Seek the advice of your insurance broker or legal counsel for assistance with questions about the scope or
meaning of the questions and how they relate to your cybersecurity practices.
Key Mitigated Threats
1. Social engineering
2. Ransomware attack
3. Loss or theft of equipment or data
4. Insider, accidental or malicious data loss
5. Attacks against network connected medical devices that may affect patient safety
37Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Appendix A: Acronyms and Abbreviaons
Table 9. Acronyms and Abbreviations
Acronym/Abbreviaon Denion
ASPR Administration for Strategic Preparedness and Response
BAA Business Associate Agreement
BYOD Bring Your Own Device
CHIP Children’s Health Insurance Program
CISO Chief Information Security Ofcer
CMS Centers for Medicare and Medicaid
DHS Department of Homeland Security
EHR Electronic Health Record
EMR Electronic Medical Record
FDA Food and Drug Administration
HHS Department of Health and Human Services
HIPAA Health Insurance Portability and Accountability Act
HITECH Health Information Technology Economic and Clinical Health Act
HMO Health Maintenance Organization
HPH Healthcare and Public Health
ICU Intensive Care Unit
INFOSEC Information Security
IoT Internet of Things
IPS Intrusion Prevention Systems
IR Incident Response
IRP Incident Response Plan
ISAC Information Sharing and Analysis Center
ISAO Information Sharing and Analysis Organization
IT Information Technology
ITAM Information Technology Asset Management
MAC Media Access Control
MACRA Medicare Access and the Children’s Health Insurance Program
Reauthorization Act
MFA Multi-Factor Authentication
MSP Managed Service Provider
MSSP Managed Security Service Provider
NIST National Institute of Standards and Technology
OCIO Ofce of the Chief Information Ofcer
OCR Ofce for Civil Rights

Appendix A: Acronyms and Abbreviations
38Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Acronym/Abbreviaon Denion
ONC Ofce of the National Coordinator (for Healthcare Technology)
PACS Pictures Archiving and Communication Systems
PCI-DSS Payment Card Industry Data Security Standard
PH-ISAC Population Health Information Sharing and Analysis Center
PHI Protected Health Information
PII Personally Identiable Information
RA Risk Assessment
RDP Remote Desktop Protocol
RFI Request for Information
ROM Read Only Memory
SAMHSA Substance Abuse and Mental Health Services Administration
SAT Security Awareness Training
SSN Social Security Number
US-CERT United States Computer Emergency Readiness Team
VOIP Voice Over Internet Protocol
VPN Virtual Private Network
WLAN Wireless Local-Area Network
39Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
Appendix B: References
“Back to Basics: Multi-Factor Authentication.” NIST Information Technology Laboratory/Applied
Cybersecurity Division. February 16, 2022. https://www.nist.gov/itl/applied-cybersecurity/tig/back-
basics-multi-factor-authentication.
“Bad Practices.” Cybersecurity & Infrastructure Security Agency (CISA). https://www.cisa.gov/
BadPractices.
Bartock, Michael et al. “NIST Special Publication 800-184: Guide for Cybersecurity Event Recovery.”
National Institutes of Standards and Technology (NIST). December 2016. https://nvlpubs.nist.gov/
nistpubs/SpecialPublications/NIST.SP.800-184.pdf.
“Business Associates.” HHS Ofce for Civil Rights. May 24, 2019. https://www.hhs.gov/hipaa/for-
professionals/privacy/guidance/business-associates/index.html.
“Circular No. A-11.” Executive Ofce of the President Ofce of Management and Budget (OMB). Section
260. August 2022. https://www.whitehouse.gov/wp-content/uploads/2018/06/a11.pdf.
“CommHIT Information Sharing & Analysis Centers.” CommunityHealth IT. https://www.
communityhealthit.org/isacs/.
“Cybersecurity for Small Business: Cyber Insurance.” Federal Trade Commission (FTC). https://www.ftc.
gov/tips-advice/business-center/small-businesses/cybersecurity/cyber-insurance.
““How to Recognize and Avoid Phishing Scams.” Federal Trade Commission. https://www.ftc.gov/news-
events/topics/identity-theft/phishing-scams.
“Cybersecurity for Small Business: Vendor Security.” Federal Trade Commission. https://www.ftc.gov/
tips-advice/business-center/small-businesses/cybersecurity/vendor-security.
“Data Breach Response: A Guide for Business.” Federal Trade Commission (FTC). February 2021. https://
www.ftc.gov/tips-advice/business-center/guidance/data-breach-response-guide-business.
Fair, Lesley. “Ransomware Risk: 2 Preventive Steps for Your Small Business.” Federal Trade Commission.
November 5, 2021. https://www.ftc.gov/news-events/blogs/business-blog/2021/11/ransomware-
risk-2-preventive-steps-your-small-business.
“FAQ 570: Does HIPAA permit health care providers to use e-mail to discuss with their patients?” HHS
Ofce for Civil Rights. July 26, 2013. https://www.hhs.gov/hipaa/for-professionals/faq/570/does-
hipaa-permit-health-care-providers-to-use-email-to-discuss-health-issues-with-patients/index.html.
“Free Cybersecurity Services and Tools.” Cybersecurity & Infrastructure Security Agency (CISA). https://
www.cisa.gov/free-cybersecurity-services-and-tools.
“Gartner Peer Insights: Reviews Organized by Markets.” Gartner LLC. https://www.gartner.com/reviews/
markets.
“Guidance on Risk Analysis.” HHS Ofce of Civil Rights (OCR). July 22, 2019. https://www.hhs.gov/hipaa/
for-professionals/security/guidance/guidance-risk-analysis/index.html.
Health-ISAC. https://h-isac.org/.
“Health Sector Cybersecurity Coordination Center (HC3).” U.S. Department of Health and Human
Services (HHS). March 31, 2022. https://www.hhs.gov/about/agencies/asa/ocio/hc3/index.html.
Appendix B: References
40Technical Volume 1: Cybersecurity Practices for Small Healthcare Organizations |
How to Implement Cybersecurity Workforce Training: Cybersecurity Workforce Training for Small
Healthcare Organizations. HHS 405(d) program. https://405d.hhs.gov/Documents/405d-howto-
cyberworkforcetraining-small.pdf.
“How to Recognize and Avoid Phishing Scams.” Federal Trade Commission. May 2019. https://www.
consumer.ftc.gov/articles/how-recognize-and-avoid-phishing-scams.
KLAS Research. https://klasresearch.com/.
Pahl, Thomas B. “Stick With Security: Secure Remote Access to Your Network.” FTC Bureau of Consumer
Protection. September 1, 2017. https://www.ftc.gov/business-guidance/blog/2017/09/stick-
security-secure-remote-access-your-network.
“Security Risk Assessment Tool.” Ofce of the National Coordinator for HealthIT. February 15, 2022.
https://www.healthit.gov/topic/privacy-security-and-hipaa/security-risk-assessment-tool.
“Avoiding Social Engineering and Phishing Attacks.” Cybersecurity & Infrastructure Security Agency
(CISA). August 25, 2020. https://www.cisa.gov/news-events/news/avoiding-social-engineering-and-
phishing-attacks.
“Small Business Cybersecurity Corner: NIST Cybersecurity Framework.” NIST. April 14, 2022. https://
www.nist.gov/itl/smallbusinesscyber/planning-guides/nist-cybersecurity-framework.
Smith, Andrew. “Cybersecurity for Small Business: Email Authentication.” Federal Trade Commission.
February 8, 2019. https://www.ftc.gov/business-guidance/blog/2019/02/cybersecurity-small-
business-email-authentication.
“Start with Security: A Guide for Business.” Federal Trade Commission. June 2015. https://www.ftc.gov/
tips-advice/business-center/guidance/start-security-guide-business#Remote.
Toth, Patricia. “Recovering from a Cybersecurity Incident: What to do Before and After.” NIST. https://
www.nist.gov/document/recovery-webinarpdf.
“Update Your Software Now.” Federal Trade Commission. June 2019. https://www.consumer.ftc.gov/
blog/2019/06/update-your-software-now.
Versel, Neil. “How easy is it to hack an infusion pump? Watch this video.” MedCity News. August 10,
2015. https://medcitynews.com/2015/08/hack-infusion-pump-video/.
“Web Browser Secure Settings.” University of California Santa Cruz Information Technology Services.
September 25, 2020. https://its.ucsc.edu/software/release/browser-secure.html.
“What Are Important Items to Include in a Vendor Contract?” Ofce of the National Coordinator for
Health IT. October 22, 2019. https://www.healthit.gov/faq/what-are-important-items-include-
vendor-contract.
